Preoperative MRI predicts outcomes in cervical spondylosis with cord compression
Preoperative Magnetic Resonance Imaging Is Associated With Baseline Neurological Status and Can Predict Postoperative Recovery in Patients With Cervical Spondylotic Myelopathy.
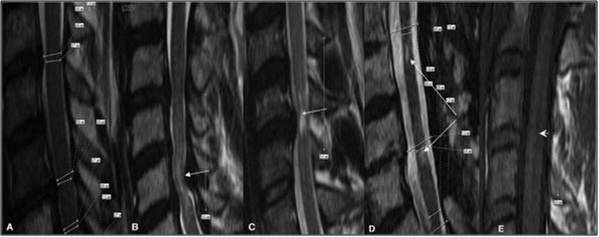
Types of MRI signal change in patients with CSM. (A) No signal change. (B) Diffuse T2 signal (open arrow). (C) Focal T2 signal (closed arrow). (D) Segmentation of T2 (double arrow). (E) Low T1 signal (arrow head). MRI indicates magnetic resonance imaging; CSM, cervical spondylotic myelopathy.
Cervical Spondylotic Myelopathy (CSM) is a major cause of disability in adults. To date magnetic resonance imaging (MRI) has not been shown to be a prognostic tool in CSM. This study looks at the baseline MRI indicators as predictors of preoperative patient status and postoperative neurological recovery administered at baseline and 1 yr after surgery.Preop and 1 yr postop measures were compared with univariate and multivariate analysis. Results: Low T1 signal change on preoperative MRI was associated with a lower mJOA (P=0.003), higher Nurick Grade (P=0.0298), decreased grip strength (P=0.0152), impaired Wt (P=0.0001) and
Wc ( P=0.0001) and poor BBS (P=0.0005) at baseline. The presence of focal high T2 signal resulted in lower mJOA scores and higher Nurick Grades as compared with diffuse T2 (P=0.0035 P=0.0079) or no T2 signal (P=0.068 and P=0.0122). In patients where the preoperative MRI showed segmentation of T2 signal, there was a significant increase in Wt and Wc and BBS (P=0.0266; P= 0.0167; P= 0.0042). Preoperative T1 signal was associated with lower postoperative grip strength (P=0.026), greater Wt (P=0.036) and Wc (P=0.009). The presence of preoperative focal T2 signal had a significant association with poorer postoperative Wt (P=0.022) and Wc (P=0.022) and Nurick scores (P=0.023). Preoperative MCC was negatively correlated with the postoperative SF-36 mental sore (P=0.013).
MRI signal changes are predictive of baseline neurological status and extent of postoperative recovery. MRI indicators of poor preoperative baseline status include presence of low T1 signal, presence of focal T2 signal and segmentation of T2 signal.
