No Benefit From Dose-Dense Chemo in Glioblastoma
 Intensified chemoradiation with temozolomide for newly diagnosed glioblastoma failed to improve survival or slow disease progression, according to results of a randomized trial.
Intensified chemoradiation with temozolomide for newly diagnosed glioblastoma failed to improve survival or slow disease progression, according to results of a randomized trial.
Patients randomized to conventional treatment with radiation therapy and temozolomide (Temodar) had a median overall survival (OS) of 16.6 months, whereas patients who received radiation and dose-dense temozolomide had a median survival of 14.9 months.
Median progression-free survival (PFS) was about a month longer with the dose-dense regimen, but the difference did not reach statistical significance, reported Mark R. Gilbert, MD, of the University of Texas MD Anderson Cancer Center in Houston, and colleagues online in the Journal of Clinical Oncology.
“This study did not demonstrate improved efficacy for dose-dense temozolomide for newly diagnosed glioblastoma multiforme, regardless of [MGMT] methylation status,” the authors concluded. “However, it did confirm the prognostic significance of MGMT (methylguanine-DNA methyltransferase) methylation. Feasibility of large-scale accrual, prospective tumor collection, and molecular stratification was demonstrated.”
A substudy within the trial, also published in the journal, showed that dose-dense temozolomide was associated with more symptoms and with greater deterioration of global health and motor function as compared with the standard regimen.
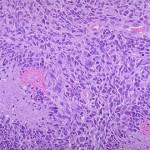
The current standard of care for glioblastoma is surgery or radiotherapy with concurrent temozolomide (chemoradiation). However, prognosis remains poor, as only about a fourth of patients survive to 2 years, the authors noted.
As part of the international cooperative-group trial that established the standard for therapy, investigators obtained tumor specimens from a subset of patients to examine changes in the promoter region of MGMT DNA repair gene. Research has shown that the enzyme has a major mechanistic role in glioblastoma’s ability to develop resistance to alkylating agents, which include temozolomide.
Examination of the tumor specimens showed that methylation-mediated silencing of the promoter region of MGMT was associated with significant improvement in OS, suggesting that modulation of enzymatic activity might improve sensitivity and response to alkylating agents.
Dose-dense temozolomide schedules have been evaluated in patients with recurrent disease and in nonrandomized studies, which showed efficacy and compared favorably with that of the standard regimen without causing additional toxicity. Schedules of 7 days on/7-days-off and 21- to 28-day cycles achieved depletion of MGMT activity. Standard therapy with temozolomide is to administer the drug on five of every 28 days.
Gilbert and colleagues hypothesized that prolonged exposure to temozolomide would improve survival in newly diagnosed glioblastoma. To test the hypothesis, investigators in Europe and North American randomized 833 patients to standard-regimen temozolomide plus radiation therapy or to dose-dense temozolomide and radiotherapy.
The primary endpoint was OS; PFS and toxicity were key secondary endpoints. Median duration of follow-up was 31.5 months.
The 1.7-month difference in OS translated into a hazard ratio of 1.03, which was not statistically significant (P=0.63). The patients randomized to standard temozolomide had a median PFS of 5.5 months versus 6.7 months for the dose-dense group (HR 0.87, P=0.06).
Data on tumor methylation status was available for 762 patients. Investigators found a significant difference in survival for patients with methylated MGMT (21.2 months) versus those with unmethylated promoter gene (14 months, HR 0.58, 95% CI 0.48-0.69, P<0.001). Median PFS was 8.7 months with methylated tumors and 5.7 months with unmethylated tumors (HR 0.61, 95% CI 0.52-0.73, P<0.001).
The dose-dense regimen was associated with increased grade ≥3 toxicity (34% versus 53%, P<0.001), primarily lymphopenia and fatigue.
Dose-dense temozolomide also had a greater adverse impact on neurocognitive function, symptoms, and quality of life, Terri S. Armstrong, PhD, of the University of Texas Health Science Center at Houston, and colleagues reported in the second article.
Investigators used validated assessment instruments to evaluate the outcomes in 182 patients at baseline and after each of the planned six cycles of therapy. Baseline scores related to neurocognitive and physical function were associated with both OS and PFS. The change in the net clinical benefit (results of all tests) from baseline to cycle one also was associated with overall survival and PFS.
Patients in the dose-dense arm had greater deterioration in all components of net clinical benefit from baseline to cycle four in global health and motor function scores, overall symptom burden, overall symptom interference, and activity related symptom interference. Neurocognitive function did not differ between the groups.
“Although future trials incorporating the net clinical benefit measures are needed to validate these findings, our results strongly support making the net clinical benefit measures a component of brain tumor clinical trials,” Armstrong’s group concluded. “These net clinical benefit measures can potentially be used for stratification and also provide a dimension of treatment for efficacy that is not adequately determined by traditional measures.”
