Gene therapy opens promising alternative in the treatment of primary malignant brain tumors
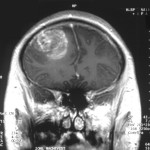 Gene therapy to protect blood stem cells from chemotherapy allows more intensive treatment of patients with glioblastoma, researchers say.
Gene therapy to protect blood stem cells from chemotherapy allows more intensive treatment of patients with glioblastoma, researchers say.
“We developed a strategy to successfully shield the marrow and blood cells and thus patients can now get this drug combination with benzylguanine and temozolomide while the marrow and blood cells are protected and shielded,” Dr. Hans-Peter Kiem from Fred Hutchinson Cancer Research Center in Seattle told Reuters Health by email.
“MGMT (methylguanine methyltransferase) in the tumor will inactivate the chemotherapy and thus make the tumor insensitive to chemotherapy,” Dr. Kiem explained. “We can reverse this by disabling MGMT and making the tumor again sensitive to temozolomide using a drug called benzylguanine. Unfortunately disabling MGMT in blood and marrow cells makes them also more sensitive to temozolomide causing low blood counts and preventing the use of this approach.”
In an effort to protect blood cells from the benzylguanine-temozolomide combination, Dr. Kiem and colleagues transplanted autologous gene-modified CD34+ cells into seven patients with newly diagnosed MGMT promoter unmethylated glioblastoma who had already received >50% surgical resection followed by radiation therapy.
Once they recovered from the stem cell transplant, patients received between two and nine cycles of adjuvant benzylguanine-temozolomide at or above the previously established maximum tolerated dose of temozolomide.
Five of the seven patients experienced myelosuppression following chemotherapy, the researcher report in the Journal of Clinical Investigation, online August 8.
But by 100 days after transplantation, only one patient had significant chemotherapy-associated myelosuppression, and this patient displayed little to no gene-modified cells in circulation at the time of chemotherapy.
In the four patients with durable gene marking throughout chemotherapy, there was a gradual decline in circulating gene-modified peripheral blood cell levels immediately following discontinuation of chemotherapy. The researchers say this suggests a potential disadvantage for gene-modified stem cells in the absence of chemoselective pressure.
One patient experienced a partial response, and six of seven patients experienced progressive disease while on chemotherapy, with a median progression-free survival of nine months. Five of these patients had demonstrated a best response of stable disease, according to the report.
Median overall survival was 20 months, with all seven patients living at one year from diagnosis. Three of seven patients were alive at two years, a significant improvement compared to similar historical patients receiving radiation therapy followed by adjuvant temozolomide. Moreover, all seven patients surpassed the median survival for patients in the same recursive partitioning analysis (RPA) class.
All patients also demonstrated greater average days gained and prevention of radial tumor growth per milligram of temozolomide administered compared with matched controls, and this was sustained for the duration of the treatment course.
As for the cost of treatment, Dr. Kiem said, “I don’t think the cost will be higher than other experimental drug therapies currently being pursued — the main cost is the genetic modification and protection of the blood cells and this is a one-time procedure.”
“This is indeed an interesting strategy especially for those patients who develop temozolomide resistance and are more likely to have severe myelosuppression as an off-target effect of (benzylguanine),” Dr. Rajiv Khanna from Royal Brisbane Hospital in Herston, Queensland, Australia, told Reuters Health by email. “Although the results are quite promising, the cohort size to too small to make any firm conclusion.”
Dr. Khanna, who has investigated other treatments for glioblastoma but was not involved in this study, added, “Immune-based therapies are emerging as powerful tool for the treatment of glioblastoma multiforme (GBM) patients. In particular, T cell therapies targeting GBM-associated antigens have provided promising results and should be considered in combination with gene therapy approach developed by these authors.”
“While lot more work will be required to provide a firm evidence for the benefit of genetically modified stem cell transplantation, this study provides an important platform for the application of this strategy for other cancers (including brain) where alkylating agent chemotherapy is a potential option,” Dr. Khanna concluded.
Source
